Ketamine
Ketamine, Psychotherapy, and Interactions with Medicines
Ketamine-assisted psychotherapy and interactions with other medications.
Updated May 8, 2024 Reviewed by Monica Vilhauer
This is the final post of a multi-part series. Click here for part 1, part 2, or part 3.
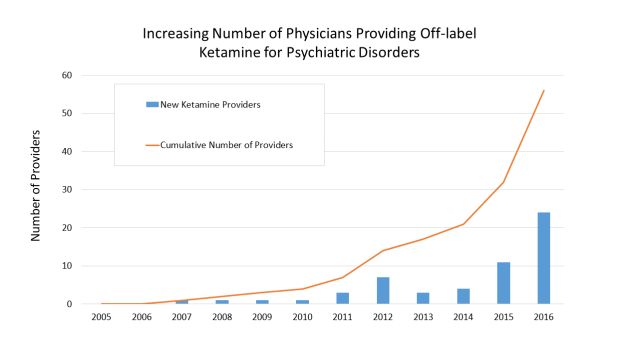
As rates of depression and anxiety have increased dramatically, people have sought therapies outside the standard regimen of oral antidepressants and talk therapy. As our research showed, beginning in the mid-2010s, more and more doctors started offering ketamine as a treatment for depression (see Figure). In 2019, the Food and Drug Administration (FDA) approved esketamine as a treatment for forms of depression that haven’t improved with standard antidepressants (like citalopram/Celexa or bupropion/Wellbutrin). With over ten years of experience with ketamine as a researcher and physician at the Yale School of Medicine, I try to answer some basic questions in this post that prospective patients often have about ketamine/esketamine.
What is “ketamine-assisted psychotherapy”?
“Ketamine-assisted psychotherapy” generally means combining ketamine with talk therapy. For a long time, researchers have noted that ketamine can increase what’s called plasticity. Plasticity (or neuroplasticity) is the brain’s ability to adapt to changing circumstances, which is critical for learning. In severe depression, plasticity is impaired, which is related to symptoms people often experience of clouded thinking and memory problems. The fact that ketamine can dramatically and rapidly increase plasticity was an incredibly exciting scientific discovery, and it is thought that this property is related to how ketamine improves depression.
Some researchers, including myself, have sought to take advantage of this therapeutic property of ketamine by pairing the treatment with psychotherapy. The thinking is, if we can make the brain more plastic, then maybe we can harness this plasticity for long-term good by engaging patients in psychotherapy. But the timing here is critical. Apparently, some clinics attempt to engage patients in psychotherapy while they are under the acute influence of ketamine. This has never made any sense to me because the best evidence shows that plasticity and learning is actually paradoxically decreased during this time period. It’s not until several hours following the conclusion of the treatment that the plasticity begins to increase. So, if you’re trying to pair ketamine with psychotherapy, the best current evidence suggests that the psychotherapy is best done at least a few hours (or more) after the conclusion of the ketamine treatment.
Can I take other antidepressants at the same time as receiving ketamine?
Esketamine, the FDA-approved form of the treatment (see my prior post on key differences between esketamine and ketamine), was designed to be taken alongside a new antidepressant. Hence, generally it makes sense to continue your antidepressant (or increase the dose or start a new antidepressant) at the same time as initiating therapy with ketamine/esketamine.
Can I stop taking my antidepressant when I start ketamine?
Sometimes, a major goal that patients have is to reduce the amount of medicine they are taking (or stop altogether). Antidepressants can have unpleasant side effects, like sexual dysfunction or weight gain, so this goal is understandable. I usually counsel patients that the first order of business is to get their depression under control, especially if it is significantly impacting their ability to function at work or at home. And this usually means continuing on an antidepressant (or starting a new one) at the same time they start ketamine/esketamine. Once we have a firm hold on the depression for at least a few months, then we can address the goal of weaning off medication. But patients should always do this in consultation with their physician, as some medications require special consideration as patients lower their dose.

What about other medications for mood and anxiety? Can I take them at the same time as ketamine/esketamine?
Benzodiazepines. Benzodiazepines (such as alprazolam/Xanax, lorazepam/Ativan, clonazepam/Klonopin) are often used in patients with depression and anxiety. Early research had suggested that if a patient was taking benzodiazepines at the time of ketamine, this might limit the effectiveness of ketamine. These reports, however, were generally small and of limited quality. As a general practice at the Yale Interventional Psychiatry Service, if a patient is taking a standing dose of benzodiazepine (as opposed to PRN, or "as needed"), we will ask them not to take that medicine the morning of ketamine/esketamine treatment. But we do not generally have patients totally discontinue benzodiazepines.
Lamotrigine/Lamictal. Patients with depression are sometimes prescribed lamotrigine/Lamictal, which is a form of mood stabilizer. Some psychiatrists have worried that, based on the proposed mechanisms of action of both lamotrigine and ketamine, that lamotrigine would interfere with the effectiveness of ketamine. This is partly based on research showing that lamotrigine can reduce the “dissociative” experience people usually have during the treatment (see my previous post for further description of what this); but as I’ve noted in these pages, this does not influence how effective ketamine is. Newer reports also indicate that there’s no reason patients need to come off their lamotrigine prior to beginning treatment with ketamine/esketamine.
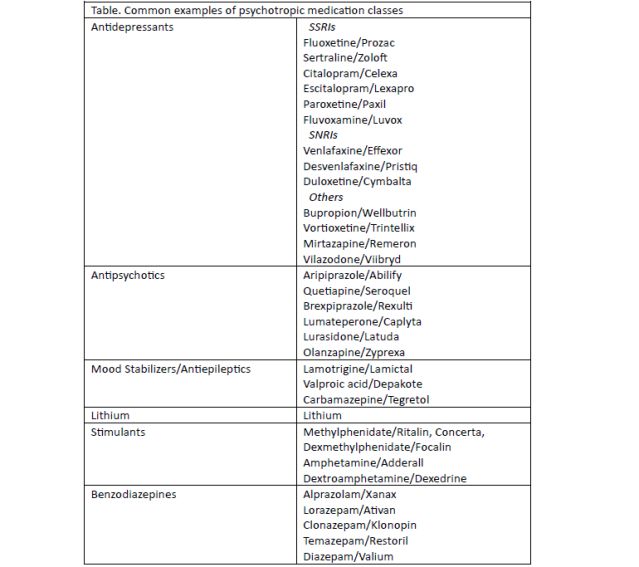
Other Medications. At the Yale Interventional Psychiatric Service, we generally allow patients to continue their antidepressants, antipsychotics, mood stabilizers/antiepileptics, and lithium. For stimulants and benzodiazepines we ask them to hold their medicine the morning before treatment. (See Table for common examples of these classes of medications.)
What is the right dose of ketamine?
Often, the dose of ketamine is measured as milligrams per kilogram (or mg/kg). This means that the actual dose of ketamine depends on how much a patient weighs. For a 70kg person (a little over 150 lbs.), a dose of 0.5mg/kg would translate into a total ketamine dose of 35mg (multiple 70kg times 0.5mg/kg). The most evidence supports using a dose of 0.5mg/kg. While it’s reasonable to increase the dose slightly if significant improvement isn’t seen after several treatments, I am cautious to go significantly higher than 0.5mg/kg (despite the fact that several clinics go well beyond this dose). At the Yale Interventional Psychiatry Service, we will cap our dose around 0.7mg/kg. The reason for caution is that, when conducting ketamine experiments in animals. If you go significantly higher, we sometimes start to see structural changes in the brain after repeated doses in ways that are concerning.
References
Efficacy of Ketamine with and without Lamotrigine in Treatment-Resistant Depression: A Preliminary Report. Joseph B, Nunez NA, Kung S, Vande Voort JL, Pazdernik VK, Schak KM, Boehm SM, Carpenter B, Johnson EK, Malyshev G, Smits N, Adewunmi DO, Brown SK, Singh B. Pharmaceuticals (Basel). 2023 Aug 16;16(8):1164.
Anand A., Charney D.S., Oren D.A., Berman R.M., Hu X.S., Cappiello A., Krystal J.H. Attenuation of the neuropsychiatric effects of ketamine with lamotrigine: Support for hyperglutamatergic effects of N-methyl-D-aspartate receptor antagonists. Arch. Gen. Psychiatry. 2000;57:270–276.
Cognitive Behavioral Therapy to Sustain the Antidepressant Effects of Ketamine in Treatment-Resistant Depression: A Randomized Clinical Trial. Wilkinson ST, Rhee TG, Joormann J, Webler R, Ortiz Lopez M, Kitay B, Fasula M, Elder C, Fenton L, Sanacora G. Psychother Psychosom. 2021;90(5):318-327.
mTOR-dependent synapse formation underlies the rapid antidepressant effects of NMDA antagonists. Li N, Lee B, Liu RJ, Banasr M, Dwyer JM, Iwata M, Li XY, Aghajanian G, Duman RS. Science. 2010 Aug 20;329(5994):959-64.
Ketamine effects on memory reconsolidation favor a learning model of delusions. Corlett PR, Cambridge V, Gardner JM, Piggot JS, Turner DC, Everitt JC, Arana FS, Morgan HL, Milton AL, Lee JL, Aitken MR, Dickinson A, Everitt BJ, Absalom AR, Adapa R, Subramanian N, Taylor JR, Krystal JH, Fletcher PC.PLoS One. 2013 Jun 12;8(6):e65088


